Blog
Guiding ob-gyns back to evidence-based care

Guiding ob-gyns back to evidence-based care | Image Credit: © Iryna – stock.adobe.com.

In every obstetrician-gynecologist (ob-gyn) practice setting, ensuring patient safety and delivering high-quality care are foundational goals. Clinical guidelines are developed precisely for these reasons: to provide care aligned with robust evidence, derived from consensus among experts, and with clear best practices. Yet clinicians occasionally deviate from these guidelines, driven by factors ranging from clinical judgment to habitual preferences rooted in past experiences. How can leaders in different practice environments thoughtfully address these deviations, maintaining respect for clinical autonomy when needed, while guiding physicians toward evidence-based and value-oriented practice?
Physician nonadherence often emerges from a well-intentioned yet deeply personal rationale. A provider may vividly recall a rare case where their decision to diverge from standard practice appeared lifesaving or where missing a rare diagnosis resulted in a poor outcome. These powerful anecdotes shape clinical decision-making, fueling cognitive biases such as availability bias (overvaluing memorable events) or confirmation bias (seeking data that support preexisting beliefs). Furthermore, seasoned clinicians might feel confident in their expertise to the point of clinical inertia, relying more on instinct than evolving evidence-based guidelines. Such circumstances may persist with consultants in other specialties who do not frequently interact with younger pregnant patients, who thus misunderstand how pregnancy physiology alters clinical decisions.
Recognizing and addressing these underlying psychological factors is crucial to effectively guide physicians back to standard practices or foster the proper and thoughtful mindset. Simply restating guidelines or enforcing strict adherence without context or empathy rarely results in meaningful or sustained change. Instead, the most impactful strategies involve listening for the factors behind decision-making, fostering self-awareness, reinforcing education when needed, employing supportive feedback mechanisms, and carefully considering the roles of incentives and, occasionally, penalties (Table).
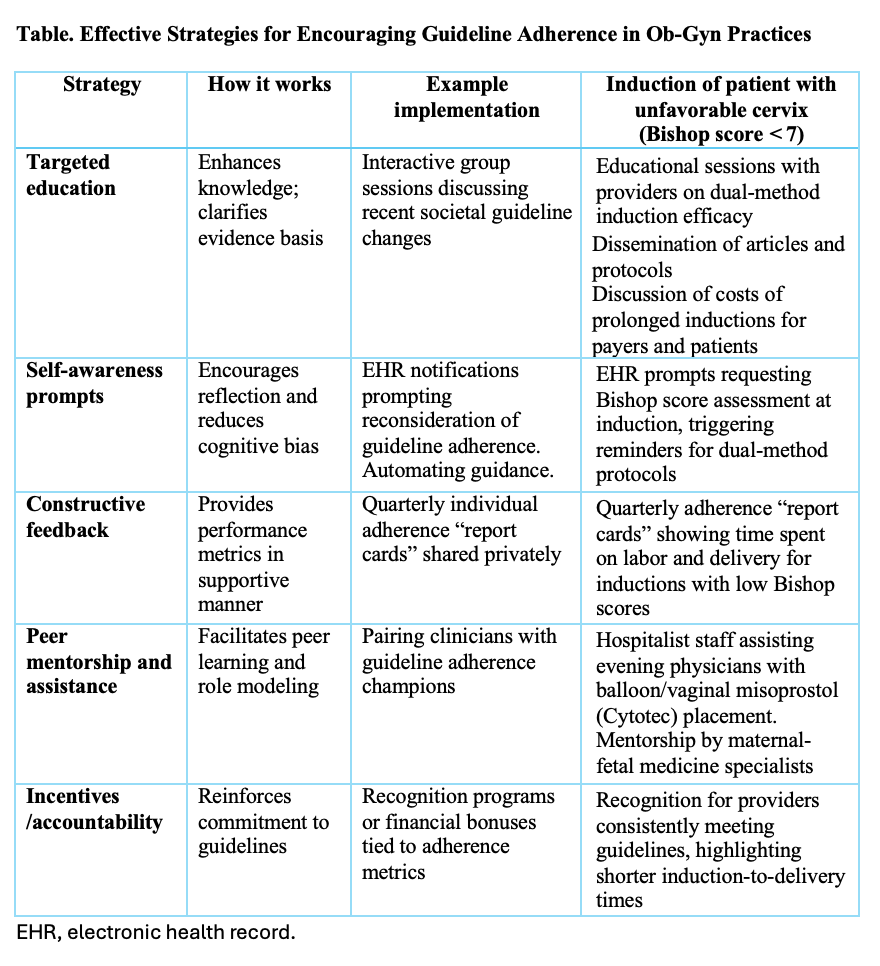
Creating opportunities for self-reflection can prompt meaningful introspection among clinicians. Integrating structured pauses in clinical workflows, such as gentle electronic health record (EHR) reminders that prompt physicians to reconsider guideline adherence, can mitigate habitual deviations. Automating processes can further reduce clinical deviation while removing burdensome work that contributes to burnout. Additionally, discussions during departmental meetings that openly acknowledge cognitive biases or past clinical errors from leadership and mentors can normalize humility and reflection, creating a culture where continual improvement is valued over perceived infallibility among all staff.
Targeted education remains a cornerstone of adherence improvement. Effective educational interventions do more than disseminate guidelines––they engage clinicians in interactive, case-based discussions, emphasizing the clinical rationale and tangible benefits of adherence. Clinicians often respond positively when presented with strong evidence of improved patient outcomes associated with specific guidelines, particularly when colleagues respected within their practice lead these discussions.
Audit and feedback, implemented constructively, can significantly influence physician behavior. Regularly providing clinicians with personalized performance data, such as adherence rates to prenatal care guidelines or cesarean delivery metrics, encourages self-assessment. Framing this feedback as collaborative rather than punitive fosters receptiveness and proactive behavior change. Highlighting areas of strength alongside areas for improvement encourages a positive response, reinforcing good practices while gently nudging clinicians toward adherence in weaker areas. Reminding physicians how guideline adherence improves quality metrics tracked by payers provides another effective reinforcement.
Structured mentorship or peer modeling further amplifies these strategies. Identifying clinicians who exemplify guideline adherence and pairing them informally or formally with those experiencing difficulties facilitates peer learning. Witnessing trusted colleagues’ successful integration of guidelines into clinical practice can dispel skepticism and inspire change, demonstrating that high-quality care and clinical autonomy are not mutually exclusive. Actively involving physicians in guideline development processes while recognizing implementation challenges provides additional learning opportunities and fosters cultural rewards for participants.
In certain scenarios, aligning incentives or applying targeted accountability measures reinforces desired behaviors. Practices might introduce modest financial incentives or recognition programs explicitly tied to adherence metrics, emphasizing organizational commitment to guideline adherence. Conversely, carefully implemented accountability frameworks—such as required peer review for consistent deviations—can reinforce seriousness while maintaining respect and collegiality.
Ultimately, fostering guideline adherence in ob-gyn settings requires a nuanced and comprehensive approach, blending psychological insight, education, mentorship, and measured incentives. An example of different strategies with a real local scenario of protocol compliance challenges is presented in the table. By approaching deviations not as mere resistance but as opportunities for reflection and growth, physician leaders and clinicians can collaboratively pursue consistently excellent, evidence-based care.












